Among the rare but serious congenital conditions that affect newborns, Gastroshiza (also spelled Gastroschisis) has drawn the attention of both medical professionals and parents worldwide. Gastroshiza is a defect in the abdominal wall of a developing baby, leading to the intestines — and sometimes other organs — being exposed outside the body.
This article provides an in-depth, clear, and medically accurate understanding of Gastroshiza, including its causes, symptoms, diagnosis, treatments, long-term outcomes, and preventive care measures.
What Is Gastroshiza?
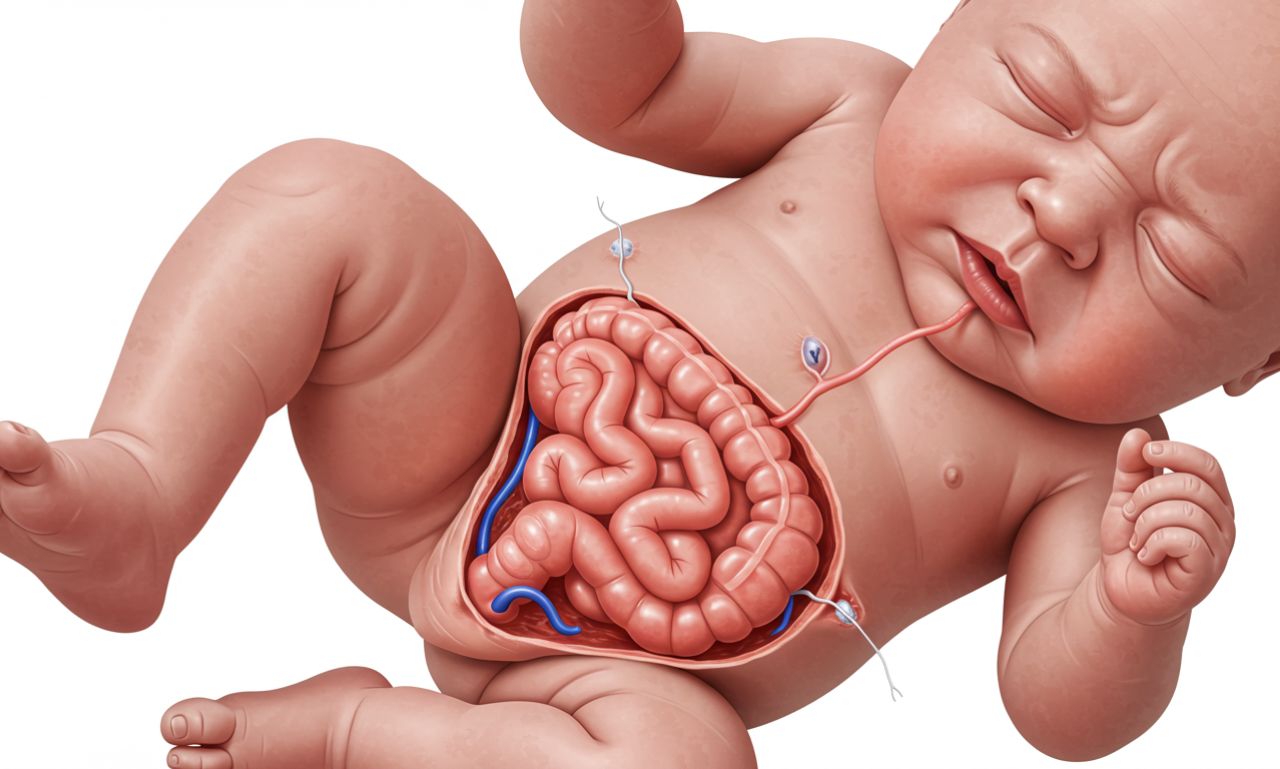
Gastroshiza is a birth defect of the abdominal wall, usually occurring to the right side of the umbilical cord. During fetal development, a small opening forms in the baby’s abdomen, allowing the intestines (and occasionally the stomach or liver) to protrude outside the body without a protective sac.
This condition develops early in pregnancy — typically within the first trimester — and requires surgical intervention soon after birth.
Key facts about Gastroshiza:
-
It occurs in approximately 1 in 2,000 to 4,000 live births worldwide.
-
The defect usually appears next to the umbilical cord but not through it.
-
Unlike other abdominal wall defects, such as omphalocele, Gastroshiza has no membrane covering the exposed organs.
Causes of Gastroshiza
The exact cause of Gastroshiza is still under study, but researchers believe it results from a combination of genetic, environmental, and developmental factors.
1. Developmental Factors
During early fetal growth, the abdominal wall forms as several tissue layers fuse. When this process fails, an opening may remain, leading to Gastroshiza.
2. Genetic Influence
While Gastroshiza is rarely inherited, certain gene-environment interactions can influence its occurrence. It’s typically not associated with chromosomal abnormalities, unlike some other congenital conditions.
3. Environmental Triggers
Some external factors have been linked to higher risk, including:
-
Maternal smoking or drug use during pregnancy
-
Young maternal age (especially under 20 years old)
-
Certain medications or exposure to toxins
-
Poor prenatal nutrition or lack of folic acid intake
Risk Factors Associated with Gastroshiza
While any pregnancy can be affected, research has identified several risk factors that increase the likelihood of Gastroshiza:
-
Young maternal age — Teen pregnancies have a higher risk rate.
-
Poor maternal nutrition — Deficiency in essential vitamins like folate.
-
Use of tobacco, alcohol, or recreational drugs.
-
Low socioeconomic conditions — Linked to limited access to prenatal care.
-
Geographic patterns — Studies show higher cases in certain regions, possibly due to environmental exposures.
Understanding these factors helps doctors and health educators design preventive strategies and targeted prenatal screening programs.
Symptoms and Characteristics of Gastroshiza
Gastroshiza is usually detected before birth during routine ultrasounds. However, once the baby is born, the condition presents very distinct and visible symptoms.
Prenatal Signs (Before Birth)
-
Ultrasound showing the intestines floating outside the fetal abdomen
-
Abnormal maternal alpha-fetoprotein (AFP) test results
-
Reduced amniotic fluid volume (oligohydramnios)
Postnatal Signs (After Birth)
-
Visible intestines outside the baby’s body, without any membrane covering
-
Possible inflammation, discoloration, or swelling of exposed organs
-
Feeding difficulties and poor digestion if other organs are affected
Because of these symptoms, immediate medical and surgical care is essential right after delivery.
Diagnosis of Gastroshiza
Early detection plays a critical role in managing Gastroshiza.
1. Prenatal Ultrasound
Modern ultrasounds can identify Gastroshiza as early as the 18th to 20th week of pregnancy. This allows parents and healthcare teams to prepare for surgical correction soon after birth.
2. Maternal Blood Tests
A higher-than-normal level of alpha-fetoprotein (AFP) in the mother’s blood can indicate potential fetal abnormalities, including Gastroshiza.
3. Postnatal Examination
After birth, the diagnosis is confirmed through a physical examination and imaging tests such as X-rays or ultrasound scans to evaluate the extent of organ involvement.
Treatment Options for Gastroshiza
1. Immediate Post-Birth Care
After delivery, the baby’s exposed intestines are covered with a sterile wrap or plastic silo to prevent dehydration, infection, and heat loss. Intravenous (IV) fluids and antibiotics are given immediately.
2. Surgical Repair
Surgery is the definitive treatment for Gastroshiza. Depending on the severity, two primary approaches are used:
a. Primary Closure
If the baby’s abdominal cavity is large enough, surgeons place the organs back inside and close the opening in a single operation.
b. Staged Repair (Silo Technique)
In more severe cases, surgeons gradually move the intestines back inside the abdomen over several days using a silo bag, followed by closing the abdominal wall once swelling subsides.
3. Post-Surgery Recovery
After surgery, the baby remains in the neonatal intensive care unit (NICU). Feeding usually begins slowly with intravenous nutrition until bowel function returns to normal.
Complications Associated with Gastroshiza
While most babies recover fully after surgery, some complications may arise during or after treatment:
-
Intestinal dysfunction or obstruction
-
Infection or inflammation of exposed organs
-
Feeding intolerance or delayed bowel movement
-
Growth and developmental delays in rare cases
However, with modern neonatal care, survival rates for Gastroshiza exceed 90%, and most infants go on to lead healthy lives.
Long-Term Outlook for Babies with Gastroshiza
The long-term prognosis depends on the extent of organ damage and the timeliness of treatment.
Most children recover well, though they may experience:
-
Minor digestive issues
-
Occasional feeding difficulties
-
Need for nutritional follow-up care
Regular pediatric monitoring ensures proper growth and developmental milestones.
Preventive Measures and Parental Awareness
While not all cases of Gastroshiza can be prevented, several steps can reduce the risk:
1. Prenatal Care
Early and consistent prenatal check-ups help detect abnormalities in time for appropriate medical planning.
2. Nutritional Health
Adequate intake of folic acid, vitamin B12, and a balanced diet supports healthy fetal development.
3. Avoid Harmful Substances
Expectant mothers should avoid:
-
Smoking
-
Alcohol consumption
-
Illicit drug use
4. Environmental Awareness
Minimizing exposure to harmful chemicals and pollutants may also lower risk factors.
5. Health Education
Public health programs that raise awareness about Gastroshiza can encourage early detection and timely medical intervention.
Emotional and Social Support for Families
The diagnosis of Gastroshiza can be emotionally overwhelming for parents. Support systems — including counseling, parent groups, and online communities — play a vital role in helping families cope before, during, and after treatment.
Many hospitals now include neonatal support teams to guide parents through each stage, offering both medical and emotional assistance.
Gastroshiza vs. Omphalocele: Understanding the Difference
Although Gastroshiza and Omphalocele may appear similar, they are distinct conditions:
| Feature | Gastroshiza | Omphalocele |
|---|---|---|
| Protective sac | Absent | Present |
| Location | To the right of the umbilical cord | Through the umbilical cord |
| Associated genetic disorders | Rare | Common |
| Treatment urgency | Immediate surgery | Planned surgical repair possible |
Recognizing these differences is crucial for accurate diagnosis and management.
Recent Advances in Gastroshiza Treatment
Modern medical research continues to improve outcomes for babies with Gastroshiza. Advances include:
-
Minimally invasive surgical techniques
-
Improved neonatal nutrition management
-
Enhanced infection control in NICUs
-
Prenatal interventions being studied to support better fetal outcomes
As medical science advances, survival rates and long-term quality of life continue to improve for children born with this condition.
Conclusion: Building Awareness and Hope Around Gastroshiza
Gastroshiza is a challenging yet manageable congenital condition when detected early and treated appropriately. Through medical innovation, preventive education, and family support, survival and recovery rates are higher than ever before.
Awareness about Gastroshiza empowers expectant mothers, healthcare providers, and communities to act swiftly — ensuring every child born with this condition has a healthy, hopeful start in life.